[su_tabs vertical=”yes”][su_tab title=”About”]
Problem
In 1986, SEARCH established a vital rate surveillance system in the rural villages of Gadchiroli and discovered that the child mortality rate was way high than that claimed by Government of Maharashtra. In this rural area with high child mortality, SEARCH conducted a field trial (1988 to 1990) of the management of pneumonia in children. We had trained village health workers (VHWs), traditional birth attendants (TBAs) and paramedics in 58 villages in the management of childhood pneumonia, resulting, by the end of the interventions, in a reduction in the infant mortality rate (IMR) from 121 to 89 per 1000 live births.

Post-1990, SEARCH faced the problem of stagnant Infant Mortality Rate (IMR) which was found to be due to high contribution of neonatal mortality and lack of effective neonatal health care in rural Gadchiroli.
The medical fraternity’s conviction was that newborns can be treated only in Neonatal Intensive Care Unit in specialised hospitals. These hospitals were in cities and out of reach of villagers, due to a complex combination of reasons including apathy, cost, lack of roads, unscientific belief system etc. Moreover, 84% of babies in villages of India were home delivered, under rampant unsanitary and hazardous living conditions. There was no community-based research data to gauge the magnitude of the problem and causes of death during the neonatal period. Hence, we conducted an observational study and collected the natural history of 763 live births, between 1995 and 1996, the world’s first study showing the prime causes of the neonatal deaths were sepsis and asphyxia.
Solution
SEARCH conceived the innovative idea of a home based newborn health care and decided to provide neonatal care in the home of the mother and newborn. We chose 39 rural villages in Gadchiroli for active intervention under this new field trial. Another 47 villages were selected where we did not intervene for sake of comparison. We selected 39 Village Health Workers – Arogya-doots – one woman from each village, and trained them in essential newborn care including monitoring (measuring temperature, weight, breath rate etc) health of the newborn during home visits on specified days, identification of high-risk babies, special care for high-risk babies, diagnosis and management of morbidities including life-threatening morbidities.

On completion of this community-based training, ten leading paediatricians from all over the country were invited to Shodhagram to examine the Arogyadoots and certify their competency. Late Dr Meharban Singh, the doyen of neonatology in India, Professor and Head of Paediatrics and Neonatal Division, All India Institute of Medical Sciences, New Delhi, commended saying,
“These ordinary looking women of Gadchiroli – these village health workers – know more about neo-natal care than the medical graduates of the All India Institute of Medical Science.”

Health Education in field.
Our Female Arogyadoots provided the following 6 interventions:
- Health Education of mothers and their care seekers for behaviour change and inducing care seeking.
- Attending home delivery: with Traditional birth Attendants.
- Care of the baby at birth including management of birth asphyxia if necessary and identification of high-risk babies.
- Home visits to monitor the health of the mother and newborn and support the mother in newborn care.
- Provide special additional care to high-risk babies.
- Management of newborn sickness including life-threatening ones eg. sepsis with oral and injectable antibiotics.
A maternal component too was added in 2008.

Outcome
By 1998, the third year of the intervention, 93 percent of newborns in the intervention area were receiving home-based care. While the NMR in the control area remained at around 60 per 1,000 live births, the NMR in the intervention area dropped from 62 to 25 per 1,000 live births — a 62 percent reduction compared to the control area. The IMR was also reduced by nearly half to 39.
Other effects:
- Beliefs and behaviours of mothers about newborn care improved significantly.
- The incidence of various newborn morbidities (especially infections, breastfeeding problems, hypothermia and mild birth asphyxia) declined overall by 49 percent.
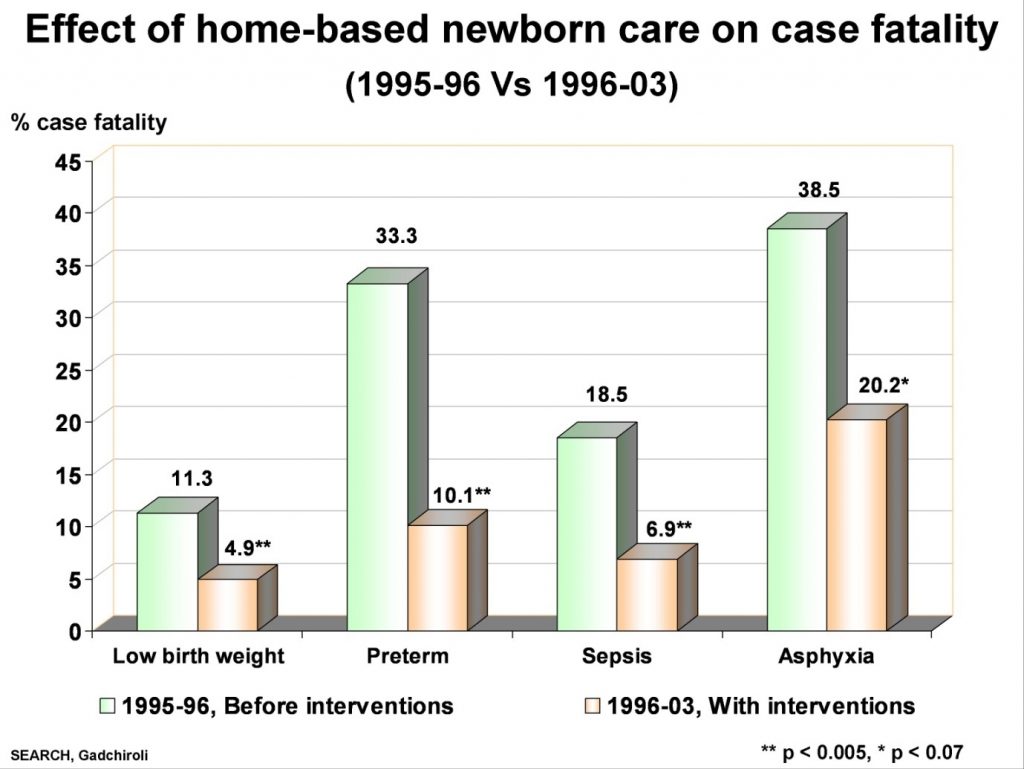
- Case fatality dropped steeply in the preterm, low birth weight newborns by nearly 60 percent as well as in the newborns treated for sepsis/pneumonia.
- Maternal morbidities during labour and postpartum decreased
Policy Shaping
The world loses more than 40% of under-five children to infant and neonatal mortality. Nearly 3.3 million neonatal deaths and an equal number of stillbirths occur each year around the world. The three major causes of deaths are infections (including sepsis/pneumonia, tetanus and diarrhoea), preterm births or low birth weight, and birth injury and asphyxia. 99% of newborn and maternal deaths occur in low- and middle-income countries. Especially Africa and South Asia have shown least progress in changing the course. In developing countries nearly half of all mothers and newborns do not receive skilled care during and immediately after birth. Presently, the maternal mortality ratio in developing countries is 239 versus 12 per 100 000 live births in developed countries.

Our local actions to overcome these, have created global actions. To know more click on the links given below.
- Impact of SEARCH model of reducing infant mortality throughout India and 12 other countries.
- Pneumonia management field trial (Under five child mortality reduction).
- Scaling up SEARCH model for reducing infant mortality throughout India (ASHA, ANKUR, MANSI and other projects) and 12 other countries
- Change in Ethiopian child mortality policy
- Hidden Child Mortality (as Human Rights Issue)
[su_heading][su_highlight]Milestones-of-HBMNCC[/su_highlight][/su_heading]
[su_document url=”http://searchforhealth.ngo/wp-content/uploads/2016/05/Milestones-of-HBMNCC.pdf” width=”1540″ height=”1180″]
[/su_tab]
[/su_tabs]